Revenue management in the healthcare space has been seen as an area ripe for RPA, but the range of disparate tasks has kept actual implementation of RPA and intelligent automation solutions relatively low, with room for growth and many more healthcare leaders considering implementation in the short term, according to a new report.
Revenue management at large healthcare systems comprises payment and reconciliation, claims management, revenue capture, prior authorization, eligibility verification, patient registration and more. These tasks have been highly manual, but their complexity has made it difficult to implement automation solutions across the revenue cycle, said The Promise of Robotic Process Automation and Artificial Intelligence in Revenue Cycle Management, a study by Waystar and The Health Management Academy.
For claims management, the study of healthcare leaders found around 40 percent currently using RPA or AI-based automation solutions for claims management, while 28 percent said they have automated payment posting and reconciliation and also eligibility verification. On the low end, only six percent have been able to apply RPA solutions to patient registration, and 10 percent to revenue capture.
“Patient registration quality assurance may have a higher level of complexity due to the variability of patient inputs on forms,” the report’s authors wrote. “As a result, it is less repetitive and less conducive to automation at this time. As organizations continue to standardize these more complex processes, RPA may become more common across the board.”
Across most areas of the revenue cycle, more than 50 percent of large healthcare systems are either currently evaluating or considering adoption of RPA/AI in the next three years, the report found.
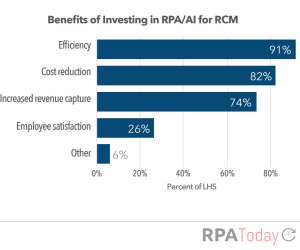
There does, however, seem to be a disconnect between the benefits healthcare companies are seeking and the ones they actually derive from RPA and intelligent automation, according to the report.
More than 80 percent of health systems using RPA/AI say their primary reason for investing in the technology was improving financial performance, but once the technology was in use, they said efficiency was the top benefit.
“[Large healthcare systems] invest in RPA/AI to alleviate margin pressure through increased net revenue capture,” the report explains. “While efficiency can contribute to margin indirectly, they may not be fully executing the workforce or workflow changes needed to maximize the revenue benefits. For example, RPA/AI in denial management can yield immediate revenue increases, but in other areas of RCM, like coding, the impact on revenue isn’t as straightforward. RPA may free up the workforce to focus on higher level work while AI can increase coding accuracy (and in turn, ensure reimbursement is sought or decrease the number of denied claims). However, these revenue benefits are indirect and take more time to realize.”
The survey also showed that the use of RPA/AI has not resulted in mass layoffs—a common fear of employees when they hear RPA is coming. Eighty-two percent of leading health systems reduced their RCM workforce following the implementation of RPA/AI, but 62 percent of executives reallocated staff to different roles while less than a quarter reported eliminating active positions.

